Cell therapy for GvHD after an allogeneic transplant
The LUMC has been involved in clinical studies using mesenchymal stromal cells (MSC) to counteract graft-versus-host disease (GvHD). GvHD can occur after allogeneic stemcell transplantation. The mesenchymal stromal cells exert anti-inflammatory and immune-modulatory properties creating a conducive environment for tissue regeneration. MSC act indirectly by promoting conditions that allow endogenous stem cells to repair the own body. LUMC researchers are currently leading the first Europe-wide randomized placebo controlled phase III trial (RETHRIM) that could provide definitive proof that MSC therapy is a successful and safe means of treating GvHD. A positive study could make MSC the standard of care in managing this debilitating disease complication.
Near future solution: gene therapy for severe combined immunodeficiency (SCID)
In patients suffering from genetic defects in the blood forming system, cells of the immune system fail to develop properly. Severe combined immunodeficiency (SCID) is the collective term for this group of rare diseases. Infants with such gene defects usually die within the first two years of life unless effective treatment is given. The curative treatment option is limited to stem cell transplantation with the risk of developing graft-versus-host disease. Recently, gene therapy using the patient’s own stem cells has become an option to treat these infants. In gene therapy, small pieces of normal DNA are inserted to correct the genetic defect in the child’s own hematopoietic stem cells. LUMC researchers are currently designing DNA vectors for the most common category of genetic defects, RAG-SCID. The project RECOMB studying gene therapy for RAG-SID started in early 2019.
Technology platform: viral vectors
The virus biology team at LUMC focusses on the development and characterization of improved viral vectors for biomedical research in general, and gene therapy. The team has four major topics of interest.
- The oncolytic virus project in which viruses that can specifically kill tumor cells are studied for cancer treatment.
- The immune evasion project which uses viral mechanisms to reduce the immune response in transplantation settings to protect transplanted tissue from destruction by the host’s immune cells.
- The gene therapy project in which healthy genetic material is introduced to fix a genetic problem at its source. The genetic material is often introduced ex vivo, meaning that the patient’s own cells are removed, edited and then re-administered after gene correction.
- Finally, the team heads the ‘LUMC viral-vector facility’, which produces viral vectors for use by LUMC researchers.
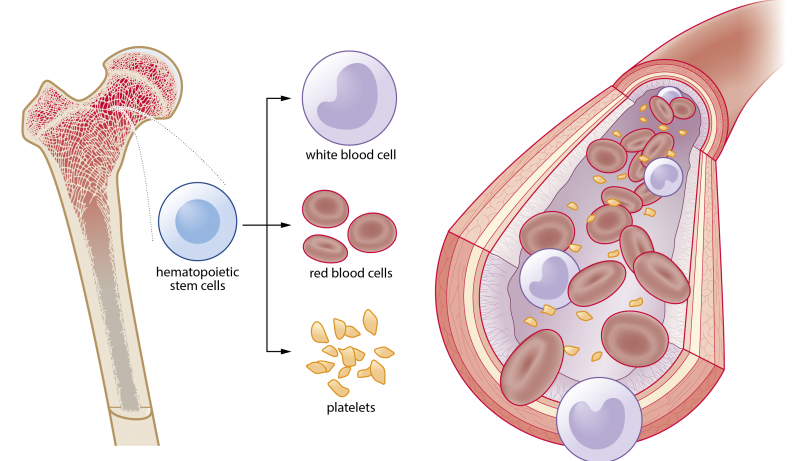
Blood function and disease
Hematopoietic stem cells residing in the bone marrow produce around 100-1000 billion blood cells each day. Our body contains roughly five litres of blood that is full of red blood cells for oxygen transport, platelets for coagulation and white blood cells that form the immune system. A properly functioning immune system identifies threats and distinguishes them from the body’s own healthy tissue. Blood and bone marrow cells are readily accessible and when isolated from a healthy donor they form a great source of cells for therapeutic use.