Cell therapy for untreatable myocardial ischemia at LUMC
Cells isolated from the bone marrow, so called bone-marrow mononuclear cells (BM-MNC) are currently used at LUMC to treat patients with untreatable myocardial ischemia. These cells are injected directly into the heart. This therapy improves the quality of life of patients as exemplified by decreased symptoms, improved exercise tolerance and cardiac function. More than 300 patients have been treated at LUMC using this cellular therapy, that is now reimbursed by health insurance companies.
The therapy does not work for all treated individuals and we are currently investigating the use of mesenchymal stromal cells (MSC) to enhance efficacy and/or the addition of exosomes, which are small vesicles produced by cells containing molecules, that could be beneficial for intrinsic cardiac repair.
Gene therapy for arrhythmias and regenerated heart valves
The long-term goal is to develop novel therapeutics for heart rhythm disturbances. Our current research in animal models indicates that it is feasible to express light-sensitive ion channels in muscle cells of the adult heart using viral vectors. Such optogenetic engineering allows precise control over electrical activity by light. Upon illumination of these cells the heart has now become able to reset itself when suffering from an arrhythmia, thereby regaining normal rhythm. These results are encouraging to further explore and refine this concept of biological auto-defibrillation to ultimately design novel, biology-driven tools that allow the heart itself to detect and neutralize pathological processes.
Other longer term goals are the generation of living heart valves. Currently used valves suffer from calcification and progressive functional degeneration. These are suitable for use in older patients, but in young children in which valves need to survive for several decades new technology is needed. At LUMC, decellularization of faulty heart valves and recellularization of these valves with healthy tissue before transplantation is studied.
Technologies; heart-on-a-chip and biological ventricular assist device
Research into drug development for heart disease employs a variety of testing systems, usually laboratory mice or murine cells. These test methods have disadvantages as murine models differ greatly from the human systems. One example is that the heart of a mouse beats 500 times a minute, while the human heart rate is on average 60 beats per minute.
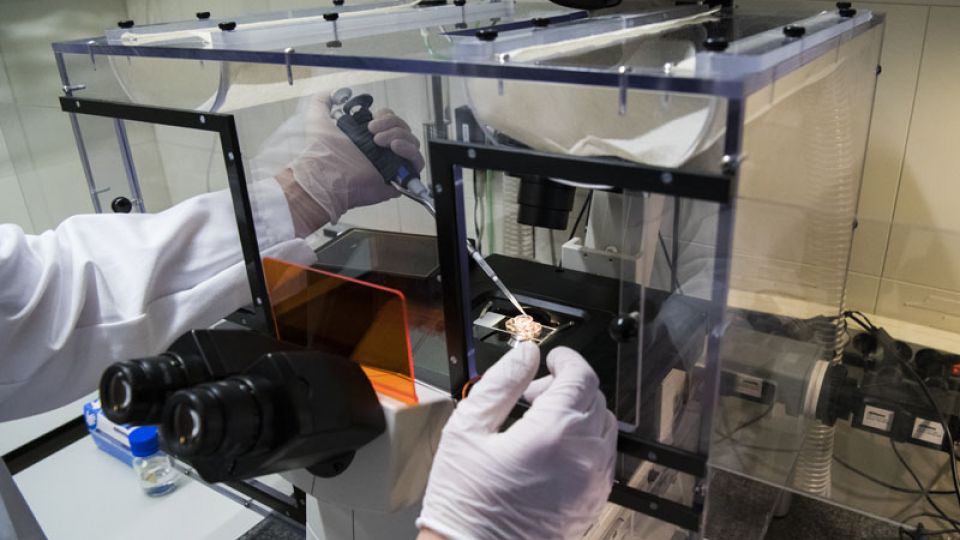
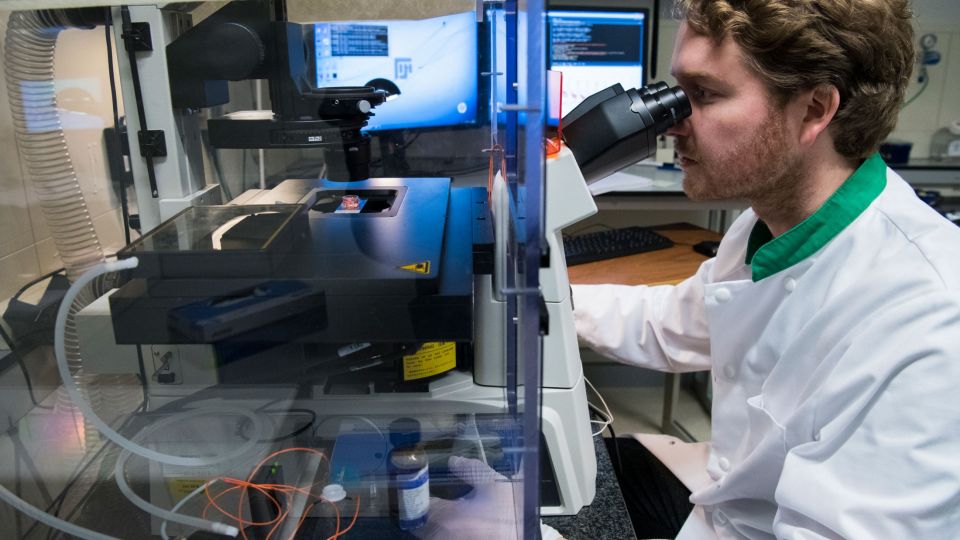
Within LUMC, new methods are devised using material from patients with heart diseases. These so-called organs-on-a-chip simulate the healthy or diseased human heart in a miniature form. The chip on which the organ is placed uses micro-channels to supply cells with blood and nutrients and allows testing of putative new drugs. This set-up allows researchers to make accurate measurements in the organ under various circumstances.
The development of these tiny organs-on-a-chip requires specific cells, induced pluripotent stem cells (iPSC). These are normal cells which are reprogrammed using forced expression of pluripotency-inducing factors to become stem cells that have the potential to form any tissue in the human body. Researchers at LUMC have used this reprogramming technique to generate organs-on-a-chip from healthy individuals, but also from patients with a (congenital) heart disease. Comparing healthy miniature hearts with diseased counterparts will generate a wealth of knowledge on heart diseases. Furthermore, it will allow for the identification of better, new therapeutics and will also lead to a significant reduction in the number of laboratory animals needed to carry out scientific medical and pharmaceutical research.
Next to the use of iPSC-derived heart tissue, LUMC is also working on a novel method for cell production using reversible cell immortalization. This unique technique should allow for the production of large quantities of a wide variety of human cells for toxicity screening and disease modelling. These cells, or the iPSC-derived heart cells, could be used for the construction of a biological ventricular assist device for in vivo use. This BioVAC might serve as a vehicle to repair damaged heart tissue.
Heart function and disease
The heart pumps roughly 5-6 litres of blood throughout the body, supplying nutrients and oxygen and removing carbon dioxide and other waste. A healthy heart beats 60 to 100 times a minute which is regulated by electrical signals sent across heart tissues. Cardiovascular disease (CVD) is a collective term of various afflictions of the heart. CVD is responsible for 1/3 of all deaths, making it the number one killer globally. Ischaemic heart disease is the most common form of CVD characterized by a reduced blood supply to the heart muscle. Complete obstruction of the blood supply leads to a myocardial infarction, better known as a heart attack. Another form of CVD is ventricular arrhythmia, caused by abnormal electrical signals to the heart chamber resulting in heart rhythm disturbances which may lead to sudden death.