Cell therapy after kidney transplantation
Mesenchymal stromal cells (MSC), a type of stem cell, are currently used to treat patients receiving a transplant to allow tapering of toxic immunosuppressive drugs. This reduces the chance of kidney dysfunction after transplantation and provides the transplanted kidney with a longer life-span. Using this method, we preserve the quality of the organ after transplantation.
Cell therapy to regenerated the donated kidney
To improve the quality and quantity of donor organs, we recently started a study to apply a new donor kidney pumping technique prior to transplantation in collaboration with Groningen and Rotterdam. Furthermore, we have shown that mesenchymal stromal cells (MSC) have the potential to induce regeneration of kidney tissue. To increase both the quality and quantity of donor kidneys we will use these cells ex vivo during kidney machine perfusion to revitalise the organ before transplantation. This may prevent the decline in quality of the kidney that occurs before the kidney is transplanted. We hypothesise that we can also revitalise older poor-quality kidneys that would otherwise be discarded. This will increase the donor organ pool reducing the time patients will spend on the transplant waiting list. We will perform these studies in our Organ Preservation and Regeneration unit at our LUMC Transplant Center.
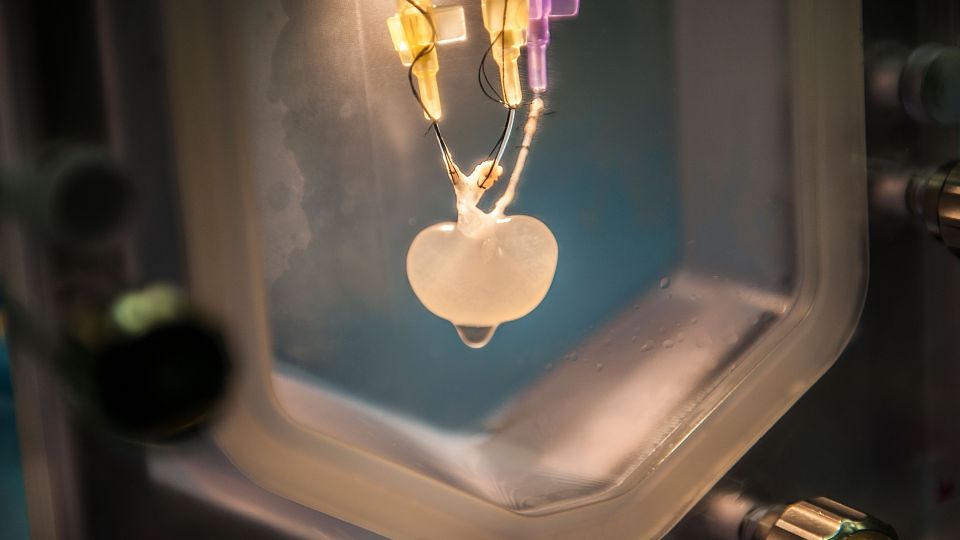
Far future: bioengineered kidney
The long-term goal is to cure patients with kidney disease without the need for life long immune suppression, and to circumvent expensive and lifestyle invasive dialysis procedure. This can only be achieved through an unlimited supply of donor organs using kidney bioengineering. Induced pluripotent stem cells (iPSc) of the patient are used, which will be turned into kidney cells. These patient specific kidney cells will be used to repopulate a kidney scaffold using an organ culture device developed at LUMC to produce a functioning kidney that is not rejected by the patient.
Kidney function and disease
Kidneys produce urine and help maintain a safe balance of fluids and minerals. In addition, they produce hormones, such as erythropoietin (EPO), to increase red blood cell production; calcitriol (Vitamin D3), to promote absorption of calcium for healthy bones; and renin, involved in monitoring and controlling blood pressure. In Europe, 10% of the population (>70 million individuals) has a degree of Chronic Kidney Disease (CKD), putting them at risk of developing kidney failure. End stage kidney disease carries a mortality rate that surpasses most cancers. Patients with less than 10% kidney function require dialysis which offers little improvement. Kidney transplantation is the only curative therapy but due to donor shortage we need alternative solutions which we are currently investigating.